Millions of Americans are covered by Medicare, yet it can be difficult to understand its regulations, particularly those pertaining to prior authorization. Medicare will pay for certain services automatically, while it will not pay for others unless they are approved. So, when is prior authorization required, and what are the implications for your medical care?
Medicare Prior Authorization: What Is It?
Medicare requires prior authorization before it will fund specific medical services or prescription drugs. The beneficiary might be responsible for the entire cost of the therapy if prior authorization is required but not received. Although this procedure guarantees medical need and helps keep expenses under control, it may also cause delays in receiving care.
Medicare Plans & Prior Authorization
When Does Medicare Require Prior Authorization?
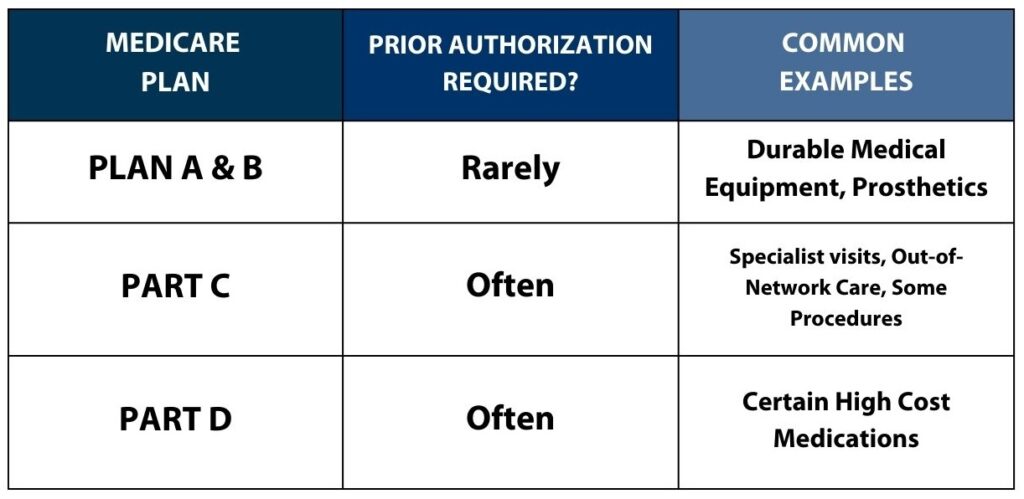
Whether you need prior authorization depends on the type of Medicare plan you have:
Traditional Medicare (Parts A & B)
- Rarely requires prior authorization for most services.
- Exceptions include prosthetics and durable medical equipment like wheelchairs or oxygen supplies.
- Beneficiaries can usually see specialists, visit hospitals, and receive care across state lines without pre-approval.
Medicare Advantage (Part C)
- Frequently requires prior authorization for specialist visits, out-of-network care, hospital services, and certain procedures.
- Rules vary by plan, so enrollees should check with their provider to confirm requirements.
Medicare Prescription Drug Plans (Part D)
- Often requires prior authorization for specific medications.
- Certain high-cost drugs or treatments may need approval before coverage applies.
Why Does Medicare Require Prior Authorization?
The Centers for Medicare & Medicaid Services (CMS) enforces prior authorization to:
✔ Ensure only necessary and appropriate procedures are approved.
✔ Prevent fraud and billing errors that increase Medicare costs.
✔ Confirm that services meet Medicare’s coverage and coding guidelines.
However, critics argue that prior authorization can delay necessary treatments, especially for home health services and chronic care patients.
How to Check If You Need Prior Authorization
Since each plan has different rules, here’s how to find out if prior authorization is required:
- Review your Medicare plan documents for a list of pre-approved services.
- Visit your plan provider’s website for up-to-date prior authorization requirements.
- Call your insurance provider directly to confirm if approval is needed.

How to Request Medicare Prior Authorization
If your service requires prior authorization, follow these steps:
- Contact your healthcare provider – They will submit the request on your behalf.
- Use your plan’s online portal – Many providers, like Select Health, offer digital tools for tracking requests.
- Submit a request through Medicare.gov – If your plan allows, you can send forms directly to Medicare.
Key Takeaways
- Traditional Medicare (Parts A & B) rarely requires prior authorization, except for some equipment and specialized services.
- Medicare Advantage (Part C) frequently requires prior authorization for specialist visits, hospital stays, and certain treatments.
- Medicare Part D often requires prior authorization for specific prescription drugs.
- Check your plan documents, website, or call your provider to confirm if prior authorization is needed.
- Requesting prior authorization can be done through your healthcare provider, your plan’s online portal, or Medicare.gov.
Understanding prior authorization requirements can help you avoid unexpected costs and delays in care. Always check in advance to ensure your medical services and prescriptions are covered
