Three Key Points about Medicare Advantage Special Needs Plans (SNPs)
- Designed for Specific Populations: These plans are tailored for individuals with specific health conditions or those who meet certain eligibility criteria, such as having both Medicare and Medicaid, residing in an institution like a nursing home, or having chronic or disabling conditions.
- Targeted Benefits and Services: SNPs offer benefits and services customized to meet the unique healthcare needs of their target population, including prescription drug coverage, care coordination, and disease management programs.
- Limited Enrollment Periods: Enrollment is typically limited to individuals who meet the specific eligibility criteria, and they can only join or switch plans during certain enrollment periods.
What Are Special Needs Plans?
Medicare Advantage Special Needs Plans are a type of Medicare Advantage Plan designed to provide targeted care for individuals with particular health needs. Unlike traditional Medicare Advantage Plans, SNPs are limited to certain groups of beneficiaries, and they offer more focused benefits and services to address their specific healthcare requirements. There are three main types of SNPs:
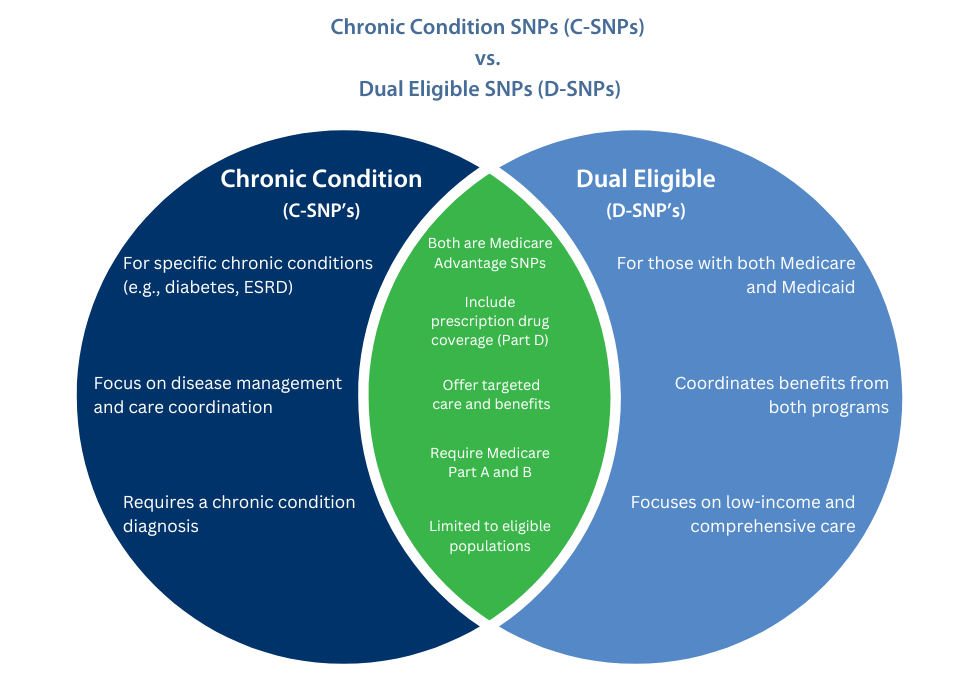
- Chronic Condition SNPs (C-SNPs): These plans cater to beneficiaries with specific chronic conditions, such as diabetes, heart failure, end-stage renal disease (ESRD), and other chronic illnesses.
- Dual Eligible SNPs (D-SNPs): These plans are for individuals who qualify for both Medicare and Medicaid, offering comprehensive benefits that coordinate both programs.
- Institutional SNPs (I-SNPs): These plans serve individuals residing in institutions, like nursing homes or long-term care facilities, providing specialized care and support.
Who May Qualify?
To be eligible for a Medicare Advantage Special Needs Plan, individuals must meet the specific criteria set by each type of SNP:
– C-SNPs: Beneficiaries must have the specific chronic condition targeted by the plan.
– D-SNPs: Eligible individuals must qualify for both Medicare (Part A and Part B) and Medicaid.
– I-SNPs: Enrollees should reside in an institution like a nursing home for at least 90 consecutive days.
How is a Medicare Advantage Special Needs Plan Different from Other Medicare Advantage Plans?
Medicare Advantage Special Needs Plans differ from other Medicare Advantage Plans in several ways:
– Targeted Population: SNPs are designed for specific groups of beneficiaries, while other Medicare Advantage Plans are open to all Medicare beneficiaries.
– Specialized Benefits: SNPs offer tailored benefits and services to address the unique healthcare needs of their target population.
– Limited Enrollment: Enrollment in SNPs is restricted to eligible individuals, and they can only join or switch plans during specific enrollment periods.
When Can You Enroll?
The enrollment periods for Medicare Advantage Special Needs Plans are similar to those for other Medicare Advantage Plans:
– Initial Enrollment Period (IEP): The IEP is the seven-month period that begins three months before your 65th birthday, includes the month of your birthday, and ends three months after your birthday month.
– Annual Enrollment Period (AEP): The AEP occurs each year from October 15th to December 7th. During this period, you can switch between different Medicare Advantage Plans, including SNPs.
– Special Enrollment Period (SEP): You may qualify for an SEP if you experience certain life events, such as moving to a new area or losing other healthcare coverage.
The Costs Associated:
The costs associated with Medicare Advantage Special Needs Plans can vary depending on the plan and the insurer. In general, beneficiaries may have to pay:
– Monthly Premiums: Some SNPs may have monthly premiums in addition to the standard Medicare Part B premium.
– Copayments and Coinsurance: You’ll likely have copayments or coinsurance for covered services, like doctor visits and prescription drugs.
– Deductibles: Some plans may have an annual deductible that you must meet before the plan starts covering costs.
It’s essential to review the specific costs and benefits of the SNP you’re interested in to understand the full extent of the coverage and expenses.
How is a Medicare Advantage Special Needs Plan Different from Medigap Plans?
Medicare Advantage Special Needs Plans and Medigap (Medicare Supplement) Plans are two different types of private insurance that work with Original Medicare. Here are the main differences:
– Coverage: Medicare Advantage Special Needs Plans provide additional benefits beyond Original Medicare, while Medigap plans help cover the out-of-pocket costs (deductibles, coinsurance, and copayments) of Original Medicare.
– Prescription Drug Coverage: Most Medicare Advantage Special Needs Plans include prescription drug coverage, whereas Medigap plans do not typically cover prescription drugs.
– Network Restrictions: Medicare Advantage Special Needs Plans often have provider networks, while Medigap plans allow you to see any doctor who accepts Medicare.
– Premiums: Beneficiaries with Medigap plans pay a separate premium in addition to their Medicare Part B premium, whereas some Medicare Advantage Special Needs Plans may have zero or low premiums.
Benefits, Limitations, and Rules Associated with Enrollment in a Medicare Advantage Special Needs Plan
Benefits:
– Customized Care: SNPs offer benefits and services tailored to the specific healthcare needs of the target population.
– Care Coordination: These plans may include care coordination services to help manage complex medical conditions effectively.
– Prescription Drug Coverage: Many SNPs include Part D prescription drug coverage as part of their benefits package.

Limitations:
– Limited Enrollment: Only individuals who meet the specific eligibility criteria for each type can enroll in the corresponding plan.
– Provider Network: Some have provider networks, meaning you may need to use in-network providers to receive full coverage.
– Enrollment Periods: Enrollment is typically restricted to certain periods, such as the Initial Enrollment Period, Annual Enrollment Period, or Special Enrollment Period.
Rules for Enrollment:
– You must have both Medicare Part A and Part B to join a Medicare Advantage Special Needs Plan.
– You can only join or switch plans during the designated enrollment periods, unless you qualify for a Special Enrollment Period due to specific life events.
– You can only be enrolled in one Medicare Advantage Plan at a time.
Most Popular Ten FAQ’s about Medicare Advantage Special Needs Plan:
What is a Medicare Advantage Special Needs Plan (SNP)?
A Medicare Advantage Special Needs Plan is a type of Medicare Advantage Plan designed for individuals with specific health conditions or qualifying characteristics.
What are the different types of Special Needs Plans (SNPs)?
There are three main types of SNPs: Chronic Condition SNPs (C-SNPs), Dual Eligible SNPs (D-SNPs), and Institutional SNPs (I-SNPs).
Who can qualify for a Medicare Advantage Special Needs Plan?
Eligibility varies depending on the type of SNP. For C-SNPs, individuals must have a specific chronic condition. D-SNPs are for those eligible for both Medicare and Medicaid, and I-SNPs serve individuals residing in institutions.
How do SNPs differ from other Medicare Advantage Plans?
SNPs are tailored for specific populations, offering targeted benefits and services. Other Medicare Advantage Plans are open to all Medicare beneficiaries.
When can I enroll in a Medicare Advantage Special Needs Plan?
You can join or switch SNPs during your Initial Enrollment Period, Annual Enrollment Period, or a Special Enrollment Period triggered by certain life events.
Are there costs associated with Medicare Advantage Special Needs Plans?
Yes, SNPs may have monthly premiums, copayments, coinsurance, and deductibles, but the specific costs vary by plan.
Can I have a Medicare Advantage Special Needs Plan and a Medigap plan at the same time?
No, you cannot have both. You must choose between a Medicare Advantage Plan and a Medigap plan, as they provide different types of coverage.
Are prescription drugs covered under Medicare Advantage Special Needs Plans?
Many SNPs include prescription drug coverage as part of their benefits package.
Are there provider network restrictions with SNPs?
Some SNPs have provider networks, requiring you to use in-network providers to receive full coverage.
Can I switch from one Medicare Advantage Special Needs Plan to another?
Yes, you can switch from one SNP to another during the Annual Enrollment Period or a Special Enrollment Period, if eligible.
Takeaways
– Medicare Advantage Special Needs Plans (SNPs) are tailored for specific populations, offering targeted benefits and services for individuals with particular health conditions or qualifying characteristics.
– There are three main types of SNPs: Chronic Condition SNPs, Dual Eligible SNPs, and Institutional SNPs.
– Eligibility, costs, and enrollment periods for SNPs vary depending on the type of SNP and individual circumstances. It’s crucial to review plan details to find the best fit for your healthcare needs.
