Senior Living Blog
Why are telehealth companies treating healthcare like the gig economy?
Telehealth has taken off. Spurred by the pandemic, many doctors in the U.S. now offer online appointments, and many patients are familiar with getting live medical advice over the internet. Given the obvious benefits, many experts have concluded that telehealth is here to stay. “It’s taken this crisis to push us to a new frontier,” […]
December 2, 2020

First blood test to help diagnose Alzheimer’s goes on sale
A company has started selling the first blood test to help diagnose Alzheimer’s disease, a leap for the field that could make it easier for people to learn whether they have dementia. It also raises concerns about the accuracy and impact of such life-altering news. Independent experts are leery because key test results have not […]
November 30, 2020

Coronavirus infections rising in New Jersey nursing homes: report
Coronavirus infections among nursing home residents are ticking higher in New Jersey as the second wave has taken effect, per a report. State health records show cases at the Dellridge Health & Rehabilitation Center in North Jersey spiked from two infections in October to seven this week, a local outlet, NorthJersey.com, reported. The incidence of cases among […]
November 17, 2020

Medicare finalizing coverage policy for coronavirus vaccine
Medicare finalizing coverage policy for coronavirus vaccine A senior Trump administration official says Medicare will cover the yet-to-be approved coronavirus vaccine free for older people under a policy change expected to be announced soon Medicare will cover the yet-to-be approved coronavirus vaccine free for older people under a policy change expected to be announced shortly, […]
November 16, 2020
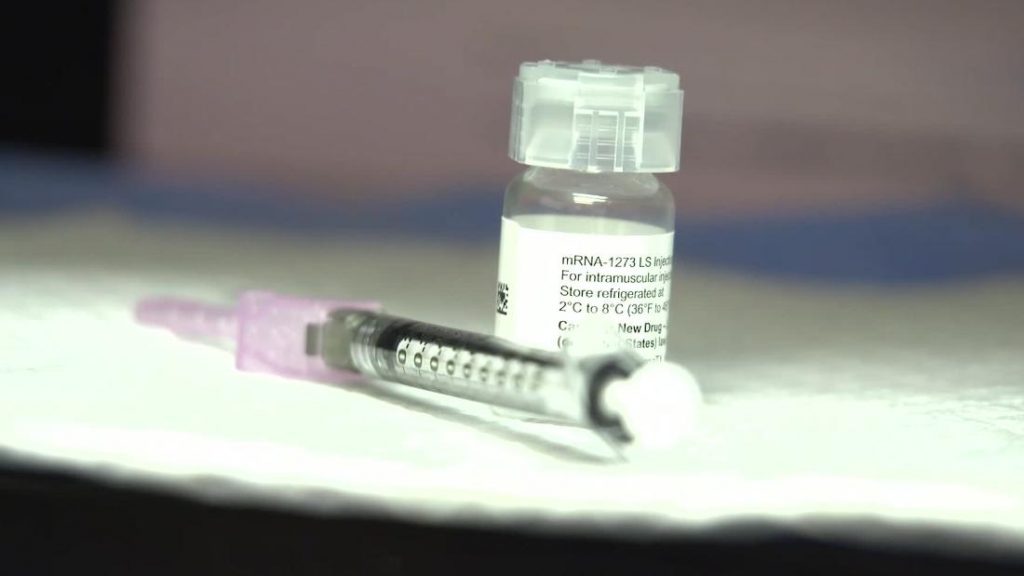
CVS, Walgreens to help distribute Covid vaccines to nursing homes
CVS, Walgreens to help distribute Covid vaccines to nursing homes The federal government has made a deal with retail pharmacies CVS and Walgreens to help distribute coronavirus vaccine — once one or more gets authorized — to long-term care facilities like nursing homes, federal officials said Friday. The two drugstore chains are the best place […]
November 16, 2020

Trump administration set to announce Medicare and Medicaid will cover Covid vaccine
Trump administration set to announce Medicare and Medicaid will cover Covid vaccine The Trump administration is set to announce as early as this week that Medicare and Medicaid will cover out-of-pocket costs for a potential coronavirus vaccine that is granted emergency use authorization, according to a person familiar with the matter. Coming days before the […]
November 16, 2020

What you need to know about at-home Covid-19 tests
Is Covid testing on your shopping list? Costco, a popular wholesale store with locations across the US, has announced that it will sell a direct-to-consumer diagnostic test for Covid-19, joining a growing list of retailers providing diagnostic tests. Kent Sepkowitz writes that even though at-home Covid-19 tests will now be available at a number of […]
November 9, 2020
Let’s Break Down The Safest Ways To Vote In The 2020 Election
Make your safe voting plan, and stick to it. Election Day is Here Americans everywhere are off to the ballots to vote in one of the biggest elections of our lives. The stakes of this year’s election couldn’t be higher, and it’s more important than ever for all eligible voters to make their voices heard […]
November 3, 2020

7 Tips To Managing Holiday Stress
Parties, shopping, cooking, cleaning, entertaining and unwelcome guests — from Christmas to New Years, the festivities present a dizzying array of demands. For many, the stress of the holidays results in fatigue, insomnia, illness, anxiety and depression, rather than peace and joy.
December 5, 2018

Better Heart Health May Mean Lower Dementia Risk In Older People
A French study of older adults found that having more modifiable cardiovascular health measures at ‘optimal levels’ was tied to lower risk of dementia. Read More… Powered by NewsAPI.org
August 23, 2018
